Prenatal ultrasound diagnosis of radial ray defects & associated anomalies at 13 weeks

21-years old primigravida presented for obstetric ultrasound at 13 weeks of gestation.
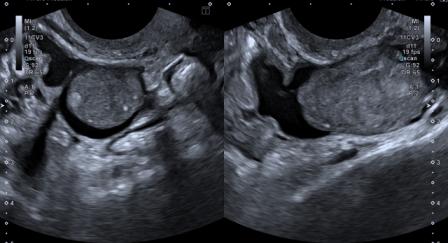
Ultrasound findings were as follows:

Figure 1: Unilateral radial aplasia, club hand and absence of thumb. Oligodactyly was bilateral.

Figure 2: Contralateral radial hypoplasia.

Figure 3: 3D ultrasound showing unilateral club foot.

Figure 4: Midline sagittal view showing micrognathia. The nasal bone is seen and nuchal translucency is 1 mm.

Figure 5: 3D ultrasound demonstrating micrognathia and low set ears.
Figure 6: Video: 3D Ultrasound clip showing structural anomalies of limbs and face described above.
Based on these findings, a working diagnosis of bilateral discordant radial ray defects with associated anomalies of the face and foot was made.
Invasive pre-natal testing was offered by CVS now or amniocentesis at 16 weeks with QfPCR / FISH for a rapid evaluation for Trisomy 21, followed by chromosomal microarray analysis and, further, if necessary, exome sequencing. However, the patient was lost to follow-up.
Radial ray defects (RRDs) are partial or complete absence of the radius and / or radial ray structures like first carpal and metacarpal bones and the phalanges of the thumb.[1]
Reported incidence is approximately 1:30,000 live births.[1]
RRDs can be isolated or associated with other structural anomalies. Most defects are unilateral and sporadic. Bilateral defects are more likely to be associated with multiple malformation syndromes.[2] The commonly associated chromosomal anomalies are trisomy 13, 18, and 22q 11.2 deletion syndromes.[1],[2]
Diagnostic testing should be offered if RRD is detected.[1]
Syndromes associated with radial ray defects [1],[2] :
VACTERL association
Holt-Oram syndrome
Cornelia de Lange syndrome
Fanconi pancytopenia syndrome
Roberts syndrome
Bollere Gerold syndrome
Thrombocytopenia with absent radius syndrome
Valproate or thalidomide exposure has been reported to be associated with RRDs.[2],[3] Autosomal dominant, autosomal recessive and X-linked inheritance have also been considered.[3] History of medication and consanguinity must therefore be sought.
3D volume rendered imaging of fetal face, limbs & spine works as a powerful supplementary tool to 2D ultrasound for better depiction of anomalies and confirmation of structural findings seen on 2D imaging.[3] It gives a superior visual impression & increases diagnostic confidence.
The 11 – 13.6 weeks scan is more than assessment of nuchal translucency and nasal bone. Careful assessment of fetal anatomy during this period can enable early detection of anomalies, which has a bearing on prognosis and management.
© Copyright Reserved
References:
1. Society for Maternal-Fetal Medicine (SMFM), Gandhi M, Rac MWF, McKinney J. Radial Ray Malformation. Am J Obstet Gynecol. 2019 Dec;221(6):B16-B18. doi:10.1016/j.ajog.2019.09.024. PMID: 31787159.
2. Yang PY, Yeh GP, Hsieh CT. Prenatal diagnosis of radial ray defects by ultrasound: A report of 6 cases. Taiwan J Obstet Gynecol. 2018 Aug;57(4):598-600. doi: 10.1016/j.tjog.2018.06.022. PMID: 30122586.
3. Kennelly MM, Moran P. A clinical algorithm of prenatal diagnosis of Radial Ray Defects with two and three dimensional ultrasound. Prenat Diagn. 2007 Aug;27(8):730-7. doi: 10.1002/pd.1770. PMID: 17533626.