Beware of this hydrosalpinx-mimic on ultrasound
A 69-year old lady was referred for abdominal ultrasound. Her complaints were abdominal pain and bleeding per vaginum since 1 week. The pain was intermittent and relieved with anti-spasmodic medication.
The patient was hemodynamically stable with normal vital parameters. The abdomen was soft and unremarkable on palpation.
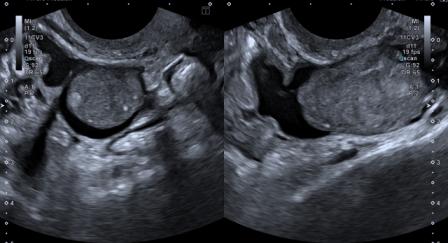
Ultrasound findings were as follows –

Figure 1: Distended endometrial cavity shows a fluid collection with mobile internal echoes.
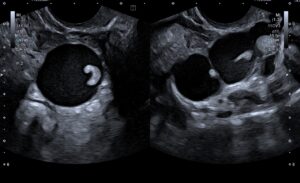
Figure 2: A lobulated cystic lesion measuring 11 x 3 cm seen in the left adnexa, suggestive of hydrosalpinx. It showed small eccentric solid nodular component along the wall, with presence of mobile internal echoes in the fluid.
Figure 3 – Video: The left adnexal lesion demonstrated.
Based on clinical presentation and ultrasound findings, a diagnosis of hematometra with left hydrosalpinx / hematosalpinx was made. Follow-up was recommended.
Patient presented for follow-up 4 months later. The collection in the endometrial cavity had resolved and endometrium measured 5 mm. The left adnexal ultrasound findings were as follows –
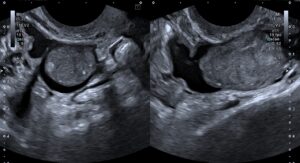
Figure 4: The hydrosalpinx appeared unchanged in size; however, the soft tissue component had increased in size, appeared lobulated and measured 6 x 2.2 cm.
Figure 5 – Video: The left adnexal lesion. Vascularity was noted in the soft tissue component on Doppler.
The interval change in the morphology of the left adnexal lesion was highly suspicious for malignant neoplasm of the fallopian tube, and thus a strong possibility of the same was raised.
Hysterectomy with bilateral salpingo-oophorectomy was performed. The appearance of the lesion is shown below:

Figure 6: The surgically excised lesion.
Histopathological analysis revealed the lesion to be primary high-grade serous adenocarcinoma of the left fallopian tube (stage pT1a).
Primary malignant neoplasm of the fallopian tube is a rare gynaecological cancer. It forms just 0.5% of all gynaecological malignancies (Schneider et al., 2000). The patients are generally post-menopausal with peak incidence in sixth decade.[1]
Parity is considered to offer some protection against the disease.[1]
The commonest tubal malignancy is serous papillary adenocarcinoma. Generally it is unilateral. CA 125 level is raised in 65-80% patients.[1],[2]
The typical symptoms of tubal malignancy, known as Latzko’s triad, consist of colicky abdominal pain, bleeding per vaginum and watery vaginal discharge.[3] The patient may give history of pain relief following the vaginal discharge. However, typical symptoms are uncommon.
Since the prognosis depends on the stage at which the disease is diagnosed, early diagnosis makes a difference. The ultrasound appearance may be as follows [1],[4] –
- An elongated tubular cystic structure with thin walls and a small eccentric solid mural nodule along the wall.
- An elongated tubular cystic structure with thin walls and a large solid component occupying part of the cystic space.
- An ovoid or oblong solid mass.
- Multilocular cystic structure with incomplete septations.
A study shows that International Ovarian Tumor Analysis (IOTA) simple rules are relatively effective in predicting tubal cancer.[5]
Treatment of primary tubal malignancy is the same as epithelial ovarian carcinoma.[2] Studies show that the prognosis of primary tubal malignancy is worse as compared to other primary gynaecological malignancies.
Pre-operative diagnosis of tubal malignancy is usually not made prior to surgery.[1] It is necessary for the radiologist to be conversant with the clinical presentation and ultrasound findings of tubal malignancy, as without a high index of suspicion, the diagnosis may be missed.
© Copyright Reserved
References:
1. Rexhepi M, Trajkovska E, Ismaili H, Besimi F, Rufati N. Primary Fallopian Tube Carcinoma: A Case Report and Literature Review. Open Access Maced J Med Sci. 2017 May 20;5(3):344-348. doi: 10.3889/oamjms.2017.044. PMID: 28698755; PMCID: PMC5503735.
2. Jaison J, Katre R, Joshi S. Primary Fallopian Tube Carcinoma: A Case Report. MIMER Med J 2017;1(2):34-36.
3. Vyas M N, Rai S, Manjeera L, Shetty D. Bilateral primary fallopian tube carcinoma with the classical clinical features: a case report. J Clin Diagn Res. 2013;7(4):726-728. doi:10.7860/JCDR/2013/4518.2894.
4. Ludovisi M, De Blasis I, Virgilio B, Fischerova D, Franchi D, Pascual MA et al. Imaging in gynecological disease (9): clinical and ultrasound characteristics of tubal cancer. Ultrasound Obstet Gynecol. 2014 Mar;43(3):328-35. doi: 10.1002/uog.12570. PMID: 23893713.
5. Tongsong T, Wanapirak C, Tantipalakorn C, Tinnangwattana D. Sonographic Diagnosis of Tubal Cancer with IOTA Simple Rules Plus Pattern Recognition. Asian Pac J Cancer Prev. 2017 Nov 26;18(11):3011-3015. doi: 10.22034/APJCP.2017.18.11.3011. PMID: 29172273; PMCID: PMC5773785.