The lurking stranger in fetal echo: persistent left superior vena cava

I discuss here a fetal cardiovascular condition that we commonly come across –persistent left superior vena cava (PLSVC).
The echocardiographic spectrum of findings in PLSVC has been documented below:
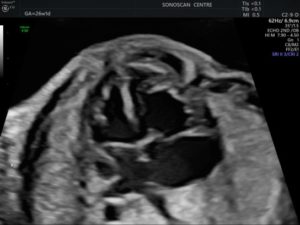
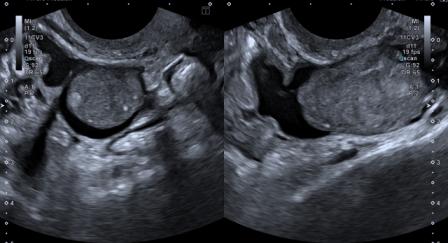
Figure 1: The 4-chamber view shows LSVC at the left border of left atrium. Cardiac chambers are normal in size.
Figure 2 – video: In the left parasagittal plane, the LSVC is seen draining into the coronary sinus.
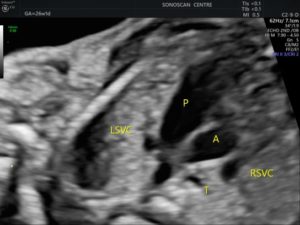
Figure 3: This 3VTV shows a fourth vessel to the left and anterior of pulmonary artery, which is the PLSVC. Both LSVC and RSVC are present.
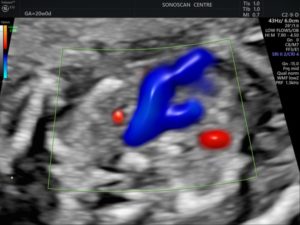
Figure 4: The same 3VTV as above, seen on colour Doppler.
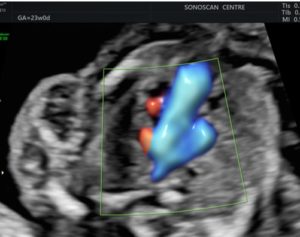
Figure 5: In another 3VTV, the third vessel is seen situated to the left of the pulmonary artery. That’s the LSVC. The RSVC is absent.
Figure 6 – video: The LSVC (as seen in Figure 5) drains into the right atrium through a dilated coronary sinus.
Figure 7 – video: Since the RSVC is absent (as seen in Figure 5), the brachiocephalic vein is present, but the direction of flow is from right to the left, as seen on colour Doppler.
PLSVC is the most common variant of anomalous systemic venous return in adults, thought to be the result of in-utero failure of regression of the left anterior & common cardinal veins. The result is presence of bilateral SVCs. Occasionally, the right SVC is absent and the venous return from the upper body enters the coronary sinus via LSVC, and thence to the right atrium. In the majority of cases, PLSVC has no clinically significant hemodynamic implications.[1]
RV/LV and PA/Ao ratios of PLSVC fetuses can be significantly higher than normal. These differences appear to diminish with gestational age.[2] In 92% cases, PLSVC drains into the RA, and in 8% in the LA if the coronary sinus is partially or completely unroofed.[3]
PLSVC can be associated with cardiac and extracardiac anomalies, in which case chromosomal anomalies may also be present. A meta-analysis suggests that cardiac and extra-cardiac anomalies were seen in 60% and 31% cases respectively.[1]
Commonly associated cardiac anomalies are heterotaxy syndromes, conotruncal anomalies & coarctation of aorta.[1] Commonest extra-cardiac anomalies are single umbilical artery and umbilical vein varix.[1] Trisomy 18 and trisomy 21 are the commonly associated chromosomal anomalies. In isolated PLSVC, there is no sufficient evidence to offer prenatal testing.[1]
Since isolated PLSVC has no clinical significance, it becomes imperative to do a detail fetal anatomical survey and echocardiography when PLSVC is detected.[4]
Differential diagnosis of LSVC is a vertical vein of supracardiac total anomalous pulmonary venous connection (TAPVC). In PLSVC, flow is directed towards the heart and the left brachiocephalic vein is usually absent. In supracardiac TAPVC, the direction of flow in the vertical vein is towards the head and the brachiocephalic vein is normal sized or dilated.
© Copyright Reserved
References:
1. Gustapane S, Leombroni M, Khalil A, Giacci F, Marrone L, Bascietto F et al. Systematic review and meta-analysis of persistent left superior vena cava on prenatal ultrasound: associated anomalies, diagnostic accuracy and postnatal outcome. Ultrasound Obstet Gynecol 2016;48(6):701-708.
2. Liu X, He Y, Tian Z, Rychik J. Persistent left superior vena cava connected to the coronary sinus in the fetus: effects on cardiac structure and flow dynamics. Pediatr Cardiol 2016;37(6):1085-90.
3. Abuhamad A, Chaoui R. A Practical Guide to Fetal Echocardiography: Normal and Abnormal Hearts. 3rd Ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2015.
4. Galindo A, Gutierrez-Larraya F, Escribano D, Arbues J, Velasco JM. Clinical significance of persistent left superior vena cava diagnosed in fetal life. Ultrasound Obstet Gynecol 2007;30(2):152-161.