A very rare fetal complication due to obstructive uropathy

A 24-years old primigravida presented for ultrasound at 27w6d gestation.
The ultrasound findings were as follows:
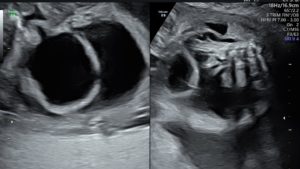
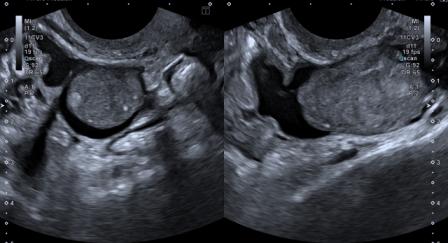
Figure 1: The fetal urinary bladder is distended and shows wall thickening. Dilated posterior urethra is seen. The mildly dilated and tortuous right ureter is visible (The left ureter was also mildly dilated; not seen here). Fetal ascites is noted.

Figure 2: Gross ascites in fetal abdomen with a clear focal defect along the dome of the distended fetal urinary bladder.
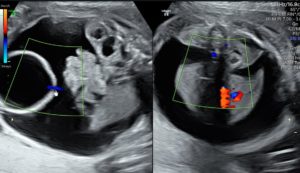
Figure 3: Colour Doppler shows a clear colour jet across the bladder wall at the site of the focal defect.
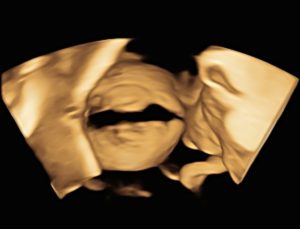
Figure 4: 3D volume rendering clearly demonstrates the rent in the urinary bladder wall.

Figure 5: Mild fullness is seen in bilateral fetal renal pelvis. No caliectasis on either side. Kidneys were otherwise normal.
There was no subcutaneous edema or pleural effusion. Rest of the fetal anatomical survey was normal. Based on the above ultrasound findings, the diagnosis arrived at was: posterior urethral valves causing bladder obstruction, with resultant bilateral hydroureter and rupture of the urinary bladder leading to fetal ascites.
The commonest cause of obstruction below the level of urinary bladder is posterior urethral valves (PUV). Less common etiologies include urethral agenesis, persistence of cloaca, anterior urethral valves and prolapsed uretrocele.[1],[2] There may be an association with chromosomal abnormalities.
The back-pressure changes due to bladder outlet obstruction can lead to bladder diverticula, reflux with hydroureter and hydronephrosis. Depending upon severity of obstruction, the resultant hydronephrosis can lead to variable degree of renal parenchymal damage, with complete loss of renal function in most severe cases. Oligohydramnios may be seen with attendant complications like pulmonary hypoplasia and limb deformities. However, antenatal rupture of urinary bladder is very rare.
Only a limited number of cases of fetal bladder rupture have been reported in the literature, with lower urinary tract obstruction as the commonest cause.[2]
Blessed et al reported spontaneous rupture of fetal urinary bladder, for which they successfully placed peritoneal amniotic shunt.[3] They also confirmed spontaneous healing of the bladder rupture on neonatal cystourethrogram. Spontaneous rupture of fetal baldder has also been reported secondary to maternal intake of certain drugs such as fentanyl, furosemide, diltiazem, aminophylline and morphine sulfate.[4]
When the amniotic fluid volume is normal, megacystis-microcolon-intestinal hypoperistalsis syndrome should be considered in differential diagnosis of a large fetal bladder.[1]
Decision regarding intervention for obstructed fetal bladder is based upon factors like underlying etiology, other anomalies, chromosomal status, the gestational age, the degree of obstruction and quality of renal function.[1],[2]
© Copyright Reserved
References:
1. Bettelheim D, Pumberger W, Deutinger, Bernaschek G. Prenatal diagnosis of fetal urinary ascites. Ultrasound Obstet Gynecol 2000;16:473-475.
2. Singh N, Tripathi R, Tyagi S, Batra A. Antepartum fetal bladder rupture leading to urinary ascites: attempt to rescue by placement of peritoneo-amniotic shunt. BMJ Case Rep 2013;2013:bcr:2013200021.Published 2013 Aug 13. doi:10.1136/bcr-2013-200021.
3. Blessed WB, Sepulveda W, Romero R, et al. Pre-natal diagnosis of spontaneous rupture of foetal bladder with colour Doppler ultrasonography. Am J Obstet Gynecol 1993;2013:1629-31.
4. Palmer E, Oliveros M, Fong J, Graham G. Medication induced fetal bladder rupture: a case report. Open J Obstet Gynecol 2011;1:17-20.